
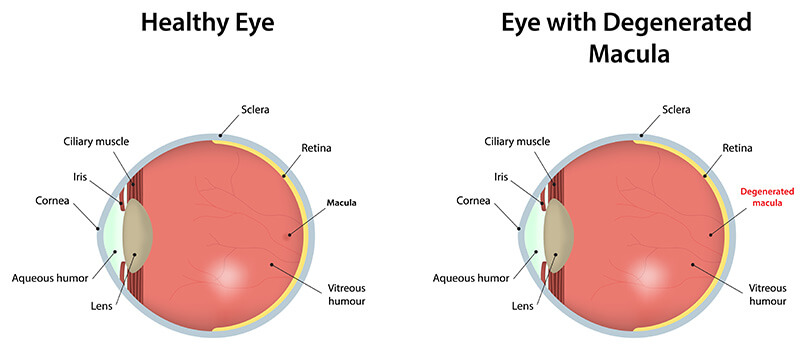
Macular degeneration effects cells in the macula, which is the part of the retina responsible for central vision. Central vision is essential for most basic tasks like reading, driving, recognizing people, etc. Thus, although macular degeneration leaves peripheral vision intact, it can be quite debilitating in its advanced state.
The disease exists in two forms, dry and wet. Dry macular degeneration is by far the most common (roughly 90% of all cases). However, it is the milder of the two forms, develops gradually and usually leads to only minor vision loss. Dry macular degeneration tends to occur when yellow fatty particles called drusen accumulate in the retina underneath the macula. This build-up results in thinning and drying-out of the macular cells.
Wet macular degeneration is less common but the vast majority of severe vision loss cases result from this form. First, abnormal blood vessels form underneath the surface of the retina. Leakage of blood and other fluids from these blood vessels permanently damage the outside cells (which detect incoming light). As these cells are damaged, vision is lost.
The primary cause of macular degeneration remains unknown. Macular degeneration typically occurs more frequently in the aging population with patients over 60. Research has shown there are many other factors such as family history, smoking, hypertension, obesity and/or a high cholesterol, high fat diet that may contribute towards the development of macular degeneration.
If you are experiencing any symptoms of macular degeneration, we encourage you to contact us today to schedule a consultation.
Unfortunately, there is no treatment for the dry form of macular degeneration. Those at high risk should schedule a checkup with their ophthalmologist at least once every one to two years, to catch the disease in its infancy. Also, it is thought that dietary supplementation of antioxidants and zinc may help to slow its development.
There is also no cure for wet macular degeneration. There are, however, several treatments designed to combat the disease. Early detection is very important because once vision is lost there is no treatment to regain it.